Can A Torn Acl Be Repaired
| Anterior Cruciate Ligament injury | |
|---|---|
 | |
| Diagram of the right human knee | |
| Specialty | Orthopedics |
| Symptoms | Audible "cleft" with pain, knee joint instability, swelling of knee[one] |
| Causes | Non-contact injury, contact injury[two] |
| Risk factors | Athletes, females[i] |
| Diagnostic method | Physical exam, MRI[i] |
| Prevention | Neuromuscular training,[3] cadre strengthening[4] |
| Handling | Braces, physical therapy, surgery[1] |
| Frequency | c. 200,000 per year (US)[2] |
An anterior cruciate ligament injury occurs when the anterior cruciate ligament (ACL) is either stretched, partially torn, or completely torn.[ane] The most common injury is a consummate tear.[1] Symptoms include hurting, an audible cracking audio during injury, instability of the genu, and joint swelling.[1] Swelling generally appears within a couple of hours.[two] In approximately 50% of cases, other structures of the human knee such as surrounding ligaments, cartilage, or meniscus are damaged.[1]
The underlying machinery ofttimes involves a rapid modify in direction, sudden end, landing afterward a bound, or direct contact to the knee.[1] It is more than common in athletes, especially those who participate in alpine skiing, football (soccer), American football game, or basketball.[ane] [v] Diagnosis is typically made by concrete examination and is sometimes supported by magnetic resonance imaging (MRI).[one] Physical examination will ofttimes show tenderness effectually the knee joint, reduced range of motion of the knee, and increased looseness of the articulation.[6]
Prevention is by neuromuscular training and core strengthening.[3] [4] Treatment recommendations depend on desired level of activity.[1] In those with depression levels of futurity action, nonsurgical management including bracing and physiotherapy may be sufficient.[1] In those with high activity levels, surgical repair via arthroscopic anterior cruciate ligament reconstruction is ofttimes recommended.[one] This involves replacement with a tendon taken from another surface area of the body or from a cadaver.[six] Post-obit surgery rehabilitation involves slowly expanding the range of motion of the joint, and strengthening the muscles around the knee joint.[i] Surgery, if recommended, is by and large not performed until the initial inflammation from the injury has resolved.[i]
About 200,000 people are affected per year in the U.s..[2] In some sports, females have a higher risk of ACL injury, while in others, both sexes are every bit affected.[5] [seven] While adults with a consummate tear accept a higher charge per unit of genu osteoarthritis, treatment strategy does not appear to alter this risk.[8]
Signs and symptoms [edit]
When an individual has an ACL injury, they are likely to hear a "pop" in their knee followed past pain and swelling. They may also experience instability in the knee joint one time they resume walking and other activities, as the ligament tin no longer stabilize the human knee articulation and keep the tibia from sliding forrad.[ix]
Reduced range of motion of the articulatio genus and tenderness along the articulation line are besides common signs of an acute ACL injury. The pain and swelling may resolve on its own; even so, the genu will remain unstable and returning to sport without treatment may result in further harm to the knee.[ane]
Causes [edit]

Causes may include:
- Changing direction apace (also known as "cutting")
- Landing from a leap awkwardly
- Coming to a sudden stop when running
- A straight contact or collision to the knee (e.g. during a football tackle or a motor vehicle collision)[1]
These movements cause the tibia to shift away from the femur rapidly, placing strain on the knee joint and potentially leading to rupture of the ACL. About 80% of ACL injuries occur without direct trauma.[ten] Adventure factors include female anatomy, specific sports, poor workout, fatigue, and playing on a turf field.[eleven]
Female predominance [edit]
Female athletes are two to 8 times more probable to strain their ACL in sports that involve cutting and jumping as compared to men who play the same detail sports.[12] NCAA information has institute relative rates of injury per 1000 athlete exposures equally follows:[ commendation needed ]
- Men'due south basketball 0.07, women'due south basketball 0.23
- Men's lacrosse 0.12, women'due south lacrosse 0.17
- Men'due south football 0.09, women'south football 0.28
The highest rate of ACL injury in women occurred in gymnastics, with a rate of injury per m athlete exposures of 0.33. Of the four sports with the highest ACL injury rates, three were women's – gymnastics, basketball and soccer.[13]
Differences between males and females identified as potential causes are the active muscular protection of the knee joint, differences in leg/pelvis alignment, and relative ligament laxity caused past differences in hormonal activity from estrogen and relaxin.[12] [14] Nascency control pills too appear to decrease the chance of ACL injury.[fifteen]
Say-so theories [edit]

Some studies have suggested that in that location are iv neuromuscular imbalances that predispose women to higher incidence of ACL injury. Female athletes are more likely to leap and country with their knees relatively direct and collapsing in towards each other, while well-nigh of their bodyweight falls on a unmarried human foot and their upper body tilts to one side.[16] Several theories take been described to further explain these imbalances. These include the ligament dominance, quadriceps dominance, leg dominance, and torso dominance theories.[ citation needed ]
The ligament say-so theory suggests that when females athletes land subsequently a jump, their muscles do not sufficiently blot the impact of the ground. As a issue, the ligaments of the knee joint must absorb the strength, leading to a higher run a risk of injury.[17] Quadriceps dominance refers to a tendency of female athletes to preferentially apply the quadriceps muscles to stabilize the human knee.[17] Given that the quadriceps muscles work to pull the tibia forward, an overpowering wrinkle of the quadriceps can place strain on the ACL, increasing risk of injury.[ citation needed ]
Leg dominance describes the observation that women tend to place more weight on 1 leg than another.[eighteen] Finally, body authorisation suggests that males typically exhibit greater command of the trunk in performance situations as evidenced by greater activation of the internal oblique musculus.[17] Female athletes are more likely to state with their upper body tilted to one side and more weight on one leg than the other, therefore placing greater rotational strength on their knees.[xix]
Hormonal and anatomic differences [edit]
Before puberty, there is no observed departure in frequency of ACL tears between the sexes. Changes in sex activity hormone levels, specifically elevated levels of estrogen and relaxin in females during the menstrual cycle, take been hypothesized equally causing predisposition of ACL ruptures. This is because they may increase joint laxity and extensibility of the soft tissues surrounding the articulatio genus joint.[12] Ongoing research has observed a greater occurrence of ACL injuries in females during ovulation and fewer injuries during the follicular and luteal phases of the menstrual bicycle.[20]
Study results have shown that female collegiate athletes with concentration levels of relaxin that are greater than 6.0 pg/mL are at four times higher run a risk of an ACL tear than those with lower concentrations.[21]
Additionally, female pelvises widen during puberty through the influence of sex activity hormones. This wider pelvis requires the femur to bending toward the knees. This bending towards the genu is referred to equally the Q bending. The boilerplate Q angle for men is 14 degrees and the average for women is 17 degrees. Steps can be taken to reduce this Q angle, such as using orthotics.[22] The relatively wider female hip and widened Q angle may lead to an increased likelihood of ACL tears in women.[23]
ACL, muscular stiffness, and strength [edit]
During puberty, sex activity hormones besides affect the remodeled shape of soft tissues throughout the body. The tissue remodeling results in female person ACLs that are smaller and will fail (i.e. tear) at lower loading forces, and differences in ligament and muscular stiffness between men and women. Women'south knees are less strong than men'southward during muscle activation. Force applied to a less stiff knee is more than likely to result in ACL tears.[24]
In add-on, the quadriceps femoris muscle is an antagonist to the ACL. Co-ordinate to a study washed on female athletes at the Academy of Michigan, 31% of female athletes recruited the quadriceps femoris musculus showtime as compared to 17% in males. Considering of the elevated wrinkle of the quadriceps femoris muscle during physical activity, an increased strain is placed onto the ACL due to the "tibial translation anteriorly".[25]
Pathophysiology [edit]
The genu joint is formed past three bones: the femur (thighbone), the tibia (shinbone), and the patella (kneecap). These basic are held together by ligaments, which are strong bands of tissue that keep the articulation stable while an individual is walking, running, jumping, etc. There are two types of ligaments in the knee: the collateral ligaments and the cruciate ligaments.[ commendation needed ]
The collateral ligaments include the medial collateral ligament (along the inside of the knee) and the lateral or fibular collateral ligament (along the outside of the genu). These 2 ligaments part to limit sideways movement of the knee.[6]
The cruciate ligaments form an "X" inside the knee joint with the inductive cruciate ligament running from the front of the tibia to the back of the femur, and the posterior cruciate ligament running from the back of the tibia to the front of the femur. The inductive cruciate ligament prevents the tibia from sliding out in forepart of the femur and provides rotational stability.[6]
At that place are also two C-shaped structures fabricated of cartilage called the medial meniscus and lateral meniscus that sit down on top of the tibia in the knee joint and serve as absorber for the bones.[1]
Diagnosis [edit]
Transmission tests [edit]
Most ACL injuries can exist diagnosed by examining the articulatio genus and comparing it to the other, non-injured knee. When a physician suspects ACL injury in a person who reports a popping sound in the knee followed by swelling, pain, and instability of the articulatio genus articulation, they tin can perform several tests to evaluate the damage to the knee. These tests include the pin-shift test, inductive drawer examination, and Lachman examination. The pivot-shift test involves flexing the knee while holding onto the ankle and slightly rotating the tibia inwards.[26] In the anterior drawer examination, the examiner flexes the knees to xc degrees, sits on the person's anxiety, and gently pulls the tibia towards him or herself.[27] The Lachman test is performed by placing i paw on the person'southward thigh and the other on the tibia and pulling the tibia forward.[28] These tests are meant to test whether the ACL is intact and therefore able to limit the forward motion of the tibia. The Lachman exam is recognized by most government as the near reliable and sensitive of the three.[29]
Medical imaging [edit]
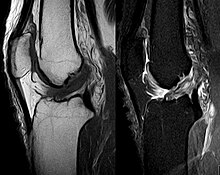
Anterior cruciate ligament tear seen on MRI. T1 left, right PDW.
Though clinical exam in experienced hands tin can exist accurate, the diagnosis is ordinarily confirmed past magnetic resonance imaging, which provides images of the soft tissues like ligaments and cartilage around the genu.[i] It may also permit visualization of other structures which may have been coincidentally involved, such as the menisci or collateral ligaments.[xxx] An x-ray may exist performed in addition to evaluate whether one of the bones in the knee joint was broken during the injury.[nine]
MRI is perchance the most used technique for diagnosing the country of the ACL, merely it is not always the most reliable technique every bit the ACL tin can be obscured past blood that fills the joint afterwards an injury.[31]
Arthrometers/Laximeters [edit]
Some other form of evaluation that may be used in case physical exam and MRI are inconclusive is laximetry testing (i.east. arthrometry and stress imaging), which involve applying a force to the leg and quantifying the resulting displacement of the human knee.[31] These medical devices basically replicate transmission tests but offer objective assessments.[32] The GNRB arthrometer, for example, is a knee arthrometer that is considered more effective than the Lachman test.[33]
Nomenclature [edit]
An injury to a ligament is called a sprain. The American University of Orthopedic Surgeons defines ACL injury in terms of severity and classifies them as Grade 1, 2, or 3 sprains.[ane] Class 1 sprains occur when the ligament is stretched slightly only the stability of the knee joint articulation is non affected. Grade 2 sprains occur when the ligament is stretched to the indicate that it becomes loose; this is also referred to as a partial tear. Grade 3 sprains occur when the ligament is completely torn into two pieces, and the knee joint is no longer stable. This is the most common type of ACL injury.[ citation needed ]
Around half of ACL injuries occur in conjunction with injury to other structures in the knee, including the other ligaments, menisci, or cartilage on the surface of the basic. A specific pattern of injury called the "unhappy triad" (also known as the "terrible triad," or "O'Donoghue's triad") involves injury to the ACL, MCL, and medial meniscus, and occurs when a lateral force is applied to the human knee while the foot is fixed on the basis.[34]
Prevention [edit]
Interest in reducing not-contact ACL injury has been intense. The International Olympic Committee, afterward a comprehensive review of preventive strategies, has stated that injury prevention programs have a measurable issue on reducing injuries.[35] These programs are especially important in female athletes who bear higher incidence of ACL injury than male athletes, and also in children and adolescents who are at high risk for a 2d ACL tear.[36] [37]
Researchers accept found that female athletes frequently land with the knees relatively direct and collapsing inwards towards each other, with most of their bodyweight on a single pes and their upper body tilting to ane side; these 4 factors put excessive strain on the ligaments on the knee and thus increment the likelihood of ACL tear.[38] [17] There is prove that engaging in neuromuscular grooming (NMT), which focus on hamstring strengthening, balance, and overall stability to reduce gamble of injury by enhancing movement patterns during high risk movements. Such programs are beneficial for all athletes, particularly adolescent female athletes.[39] [19]
Injury prevention programs (IPPs), are reliable in reducing the take a chance factors of ACL inquiries, referring to dominance theories. The ligament dominance theory reduced superlative knee abduction moment but should be more focused on prioritizing individualized, chore-specific exercises focusing on an athlete's hazard profile.[40] It is more benign than a generic program. There is an increase in hip and genu flexion angles, such as plyometrics and bound-landing tasks, which reduces the risk of quadriceps dominance. However, at that place were no changes found for meridian vGRF, which measures for "softer" landings. Unfortunately, at that place was no conclusive information on how IPPs reduces the hazard associated with leg authority theory.[40]
Treatment [edit]
Handling for ACL tears is important to:[41]
- Reduce abnormal knee movements and improve genu function
- Build trust and conviction to use the genu normally again
- Prevent further injury to the genu and reduce the risk of osteoarthritis
- Optimise long-term quality of life following the injury
Nonsurgical [edit]
Nonsurgical treatment for ACL rupture involves progressive, structured rehabilitation that aims to restore muscle strength, dynamic knee command and psychological confidence. For some, the ACL may heal without surgery during the rehabilitation process (i.east. the torn pieces re-unite to form a functional ligament).[42]
The purpose of practise treatment is to restore the normal operation of the muscular and balance system effectually the articulatio genus. Research has demonstrated that by grooming the muscles effectually the genu appropriately through exercise treatment, the body can 'larn' to command the genu once again, and despite extra movement inside the knee, the knee tin feel strong and able to withstand strength.[ citation needed ]
Typically, this approach involves visiting a physical therapist or sports medicine professional soon later injury to oversee an intensive, structured program of exercises. Other treatments may be used initially such as hands-on therapies in order to reduce hurting. The physiotherapist will human action every bit a double-decker through rehabilitation, normally by setting goals for recovery and giving feedback on progress.
Estimated non-surgical recovery timeframe is 3–half dozen months and depends on the extent of the original injury, pre-existing fettle and commitment to the rehabilitation and sporting goals. Some may not exist satisfied with the issue of not-surgical management and may opt for surgery later.[ citation needed ]
Surgery [edit]
ACL reconstruction surgery involves replacing the torn ACL with a "graft," which is a tendon taken from another source. Grafts can be taken from the patellar tendon, hamstring tendon, quadriceps tendon from either the person undergoing the procedure ("autograft") or a cadaver ("allograft"). The graft serves every bit scaffolding upon which new ligament tissue volition grow.[1]
The surgery is washed with an arthroscope or tiny photographic camera inserted inside the knee, with boosted small incisions fabricated effectually the knee to insert surgical instruments. This method is less invasive and is proven to result in less pain from surgery, less time in the hospital, and quicker recovery times than "open" surgery (in which a long incision is made down the front end of the knee and the joint is opened and exposed).[i]
The timing of ACL reconstruction has been controversial, with some studies showing worse outcomes when surgery is washed immediately subsequently injury, and others showing no divergence in outcomes when surgery is done immediately compared to when surgery is delayed.[43] [44] The American Academy of Orthopedic Surgeons has stated that there is moderate evidence to support the guideline that ACL reconstruction should occur inside five months of injury in social club to meliorate a person's office and protect the knee from further injury; withal, additional studies demand to be washed to determine the all-time time for surgery and to better understand the effect of timing on clinical outcomes.[45]
Immature athletes who take early surgical reconstruction are more than likely to return to their previous level of athletic ability when compared to those who underwent delayed surgery or nonoperative handling. They are also less likely to experience instability in their knee if they undergo early surgery.[46] [47] There are over 100,000 ACL reconstruction surgeries per year in the United States. Over 95% of ACL reconstructions are performed in the outpatient setting. The most common procedures performed during ACL reconstruction are fractional meniscectomy and chondroplasty.[48] Disproportion in the repaired knee is a possibility and has been found to have a big effect between limbs for peak vertical ground reaction forcefulness, peak knee-extension moment, and loading rate during double-limb landings, also as hateful knee-extension moment and knee free energy absorption during both double- and single-limb landings. Analysis of joint symmetry forth with movement patterns should exist a part of return to sports criteria.[49]
Rehabilitation [edit]
The goals of rehabilitation following an ACL injury are to regain knee forcefulness and movement. If an private with an ACL injury undergoes surgery, the rehabilitation process will first focus on slowly increasing the range of move of the joint, and then on strengthening the surrounding muscles to protect the new ligament and stabilize the knee. Finally, functional training specific to the activities required for certain sports is begun. It may take six or more months earlier an athlete can render to sport subsequently surgery, as it is vital to regain a sense of residuum and control over the knee in social club to prevent a second injury.[6]
Prognosis [edit]
The prognosis of ACL injury is generally good, with many people regaining part of the injured leg within months.[half-dozen] ACL injury used to exist a career-catastrophe injury for competitive athletes; however, in recent years ACL reconstruction surgery followed by physical therapy has immune many athletes to return to their pre-injury level of performance.[50]
Long term complications of ACL injury include early onset arthritis of the articulatio genus and/or re-trigger-happy the ligament. Factors that increase hazard of arthritis include severity of the initial injury, injury to other structures in the knee, and level of activeness post-obit treatment.[9] Not repairing tears to the ACL tin can sometimes crusade impairment to the cartilage inside the knee joint because with the torn ACL, the tibia and femur os are more likely to rub against each other.[1]
Unfortunately, young female person athletes have a significant risk of re-tearing an ACL graft, or tearing the ACL on the other knee after their recovery. This chance has been recorded as being nearly 1 out of every 4 young athletes.[51] Therefore, athletes should be screened for whatever neuromuscular deficit (i.east. weakness greater in one leg than another, or wrong landing form) before returning to sport.[16]
Epidemiology [edit]
At that place are around 200,000 ACL tears each twelvemonth in the United States. ACL tears newly occur in about 69 per 100,000 per twelvemonth with rates in males of 82 per 100,000 and females of 59 per 100,000.[52] When breaking downward rates based on age and sex, females betwixt the ages of 14-18 had the highest rates of injury with 227.6 per 100,000. Males betwixt the ages of nineteen-24 had the highest rates of injury with 241 per 100,000.[52]
Sports [edit]
Rates of re-rupture among college athletes were highest in male football players with fifteen per x,000, followed past female person gymnasts with 8 per x,000 and female soccer players with 5.2 per 10,000.[53]
High schoolhouse athletes are at increased risk for ACL tears when compared to not-athletes. Amidst high schoolhouse girls in the US, the sport with the highest risk of ACL tear is soccer, followed by basketball and lacrosse. In the US women's basketball and soccer experience the most ACL tears and then all other sports.[54] The highest gamble sport for high school boys in the United states was basketball game, followed past lacrosse and soccer.[55] In basketball, women are v-8 times more likely to experience an ACL tear then men.[54]
Dogs [edit]
Cruciate ligament rupture is a common orthopedic disorder in dogs. A report of insurance information showed the majority of the breeds with increased risk of cruciate ligament rupture were big or behemothic.[56]
References [edit]
- ^ a b c d e f chiliad h i j k l m north o p q r southward t u 5 west ten "Anterior Cruciate Ligament (ACL) Injuries-OrthoInfo - AAOS". orthoinfo.aaos.org. March 2014. Archived from the original on five July 2017. Retrieved 30 June 2017.
- ^ a b c d "ACL Injury: Does It Crave Surgery?-OrthoInfo - AAOS". orthoinfo.aaos.org. September 2009. Archived from the original on 22 June 2017. Retrieved 30 June 2017.
- ^ a b Hewett TE, Ford KR, Myer GD (March 2006). "Anterior cruciate ligament injuries in female person athletes: Part two, a meta-analysis of neuromuscular interventions aimed at injury prevention". The American Journal of Sports Medicine. 34 (3): 490–eight. doi:x.1177/0363546505282619. PMID 16382007. S2CID 25395274.
- ^ a b Sugimoto D, Myer GD, Foss KD, Hewett TE (March 2015). "Specific exercise effects of preventive neuromuscular grooming intervention on anterior cruciate ligament injury risk reduction in young females: meta-assay and subgroup analysis". British Journal of Sports Medicine. 49 (5): 282–9. doi:10.1136/bjsports-2014-093461. PMID 25452612.
- ^ a b Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K (December 2007). "A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee joint injury-reduction regimen". Arthroscopy. 23 (12): 1320–1325.e6. doi:10.1016/j.arthro.2007.07.003. PMID 18063176.
- ^ a b c d e f "ACL Injury: Does It Require Surgery? - OrthoInfo - AAOS". Retrieved 2018-03-22 .
- ^ Montalvo AM, Schneider DK, Yut L, Webster KE, Beynnon B, Kocher MS, Myer GD (August 2019). ""What'due south my hazard of sustaining an ACL injury while playing sports?" A systematic review with meta-analysis". British Journal of Sports Medicine. 53 (16): 1003–1012. doi:ten.1136/bjsports-2016-096274. PMC6561829. PMID 29514822.
- ^ Monk AP, Davies LJ, Hopewell S, Harris K, Bristles DJ, Cost AJ (April 2016). "Surgical versus conservative interventions for treating anterior cruciate ligament injuries". The Cochrane Database of Systematic Reviews. 4: CD011166. doi:10.1002/14651858.CD011166.pub2. PMC6464826. PMID 27039329.
- ^ a b c "ACL injury - Symptoms and causes". Mayo Clinic . Retrieved 2018-03-22 .
- ^ Dedinsky R, Baker L, Imbus S, Bowman K, Murray L (February 2017). "Exercises That Facilitate Optimal Hamstring and Quadriceps Co-Activation to Assistance Decrease Acl Injury Adventure in Healthy Females: A Systematic Review of the Literature". International Journal of Sports Physical Therapy. 12 (1): 3–15. PMC5294945. PMID 28217412.
- ^ "ACL injury - Symptoms and causes". Mayo Clinic . Retrieved 2019-xi-xv .
- ^ a b c Faryniarz DA, Bhargava Grand, Lajam C, Attia ET, Hannafin JA (2006). "Quantitation of estrogen receptors and relaxin bounden in human anterior cruciate ligament fibroblasts". In Vitro Cellular & Developmental Biology. Brute. 42 (7): 176–81. doi:10.1290/0512089.1. JSTOR 4295693. PMID 16948498. S2CID 2473817.
- ^ Hootman JM, Dick R, Agel J (April–June 2007). "Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives". Periodical of Athletic Training. 42 (ii): 311–9. PMC1941297. PMID 17710181.
- ^ Wojtys EM, Huston LJ, Schock HJ, Boylan JP, Ashton-Miller JA (May 2003). "Gender differences in muscular protection of the knee in torsion in size-matched athletes". The Journal of Bone and Articulation Surgery. American Volume. 85 (v): 782–9. doi:x.2106/00004623-200305000-00002. PMID 12728025. S2CID 42096840.
- ^ Samuelson K, Cramp EM, Sevetson EL, Fleming BC (10 October 2017). "Limited Show Suggests a Protective Association Between Oral Contraceptive Pill Use and Inductive Cruciate Ligament Injuries in Females: A Systematic Review". Sports Wellness. 9 (6): 498–510. doi:10.1177/1941738117734164. PMC5665118. PMID 29016234.
- ^ a b Hewett TE, Myer GD, Ford KR, Heidt RS, Colosimo AJ, McLean SG, et al. (Apr 2005). "Biomechanical measures of neuromuscular control and valgus loading of the human knee predict inductive cruciate ligament injury risk in female athletes: a prospective study". The American Journal of Sports Medicine. 33 (4): 492–501. doi:10.1177/0363546504269591. PMID 15722287. S2CID 31261104.
- ^ a b c d Hewett TE, Ford KR, Hoogenboom BJ, Myer GD (Dec 2010). "Understanding and preventing acl injuries: current biomechanical and epidemiologic considerations - update 2010". North American Journal of Sports Physical Therapy. 5 (4): 234–51. PMC3096145. PMID 21655382.
- ^ Pappas Eastward, Carpes FP (January 2012). "Lower extremity kinematic asymmetry in male and female athletes performing spring-landing tasks". Journal of Science and Medicine in Sport. fifteen (1): 87–92. doi:10.1016/j.jsams.2011.07.008. PMID 21925949.
- ^ a b Emery CA, Roy TO, Whittaker JL, Nettel-Aguirre A, van Mechelen Due west (July 2015). "Neuromuscular preparation injury prevention strategies in youth sport: a systematic review and meta-analysis". British Journal of Sports Medicine. 49 (13): 865–lxx. doi:10.1136/bjsports-2015-094639. PMID 26084526. S2CID 5953765.
- ^ "The female person ACL: Why is it more decumbent to injury?". Journal of Orthopaedics. thirteen (2): A1–A4. March 2016. doi:10.1016/S0972-978X(16)00023-iv. PMC4805849. PMID 27053841.
- ^ Dragoo JL, Castillo TN, Braun HJ, Ridley BA, Kennedy AC, Golish SR (Oct 2011). "Prospective correlation between serum relaxin concentration and anterior cruciate ligament tears among aristocracy collegiate female person athletes". The American Journal of Sports Medicine. 39 (ten): 2175–80. doi:10.1177/0363546511413378. PMID 21737831. S2CID 11088632.
- ^ McLean SG, Huang X, van den Bogert AJ (Oct 2005). "Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: implications for ACL injury". Clinical Biomechanics. 20 (8): 863–70. doi:x.1016/j.clinbiomech.2005.05.007. PMID 16005555.
- ^ Griffin Fifty (2008). "Gamble and Gender Factors for Noncontact Inductive Cruciate Ligament Injury". The anterior cruciate ligament : reconstruction and basic science. Saunders/Elsevier. pp. 18–27. ISBN978-1-4160-3834-four.
- ^ Slauterbeck JR, Hickox JR, Beynnon B, Hardy DM (Oct 2006). "Anterior cruciate ligament biological science and its human relationship to injury forces". The Orthopedic Clinics of Northward America. 37 (4): 585–91. doi:x.1016/j.ocl.2006.09.001. PMID 17141016.
- ^ Biondino CR (November 1999). "Inductive cruciate ligament injuries in female athletes". Connecticut Medicine. 63 (11): 657–60. PMID 10589146.
- ^ "Pivot Shift Test - Orthopedic Examination of the Knee - Concrete THERAPY Web". PHYSICAL THERAPY WEB . Retrieved 2018-03-22 .
- ^ "Anterior Drawer Test - Orthopedic Exam of the Knee - PHYSICAL THERAPY Spider web". Concrete THERAPY WEB . Retrieved 2018-03-22 .
- ^ "Lachman Test". Physiopedia . Retrieved 2018-03-22 .
- ^ van Eck CF, van den Bekerom MP, Fu FH, Poolman RW, Kerkhoffs GM (Baronial 2013). "Methods to diagnose acute anterior cruciate ligament rupture: a meta-analysis of physical examinations with and without anaesthesia". Knee Surgery, Sports Traumatology, Arthroscopy. 21 (eight): 1895–903. doi:10.1007/s00167-012-2250-9. PMID 23085822. S2CID 25181956.
- ^ MRI for Anterior Cruciate Ligament Injury at eMedicine
- ^ a b Rohman EM, Macalena JA (June 2016). "Anterior cruciate ligament assessment using arthrometry and stress imaging". Current Reviews in Musculoskeletal Medicine. 9 (2): 130–viii. doi:x.1007/s12178-016-9331-i. PMC4896874. PMID 26984335.
- ^ Robert, H.; Nouveau, S.; Gageot, S.; Gagnière, B. (May 2009). "A new knee arthrometer, the GNRB: experience in ACL complete and partial tears". Orthopaedics & Traumatology, Surgery & Research. 95 (3): 171–176. doi:ten.1016/j.otsr.2009.03.009. ISSN 1877-0568. PMID 19423416.
- ^ Ryu, Seung Min; Na, Ho Dong; Shon, Oog Jin (2018-06-01). "Diagnostic Tools for Astute Anterior Cruciate Ligament Injury: GNRB, Lachman Test, and Telos". Knee joint Surgery & Related Enquiry. thirty (2): 121–127. doi:ten.5792/ksrr.17.014. ISSN 2234-0726. PMC5990229. PMID 29554717.
- ^ O'Donoghue DH (October 1950). "Surgical treatment of fresh injuries to the major ligaments of the knee". The Journal of Bone and Joint Surgery. American Volume. 32 A (4): 721–38. doi:10.2106/00004623-195032040-00001. PMID 14784482.
- ^ Ardern CL, Ekås GR, Grindem H, Moksnes H, Anderson AF, Chotel F, et al. (April 2018). "2018 International Olympic Committee consensus argument on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries". British Journal of Sports Medicine. 52 (seven): 422–438. doi:x.1136/bjsports-2018-099060. PMC5867447. PMID 29478021.
- ^ Lang PJ, Sugimoto D, Micheli LJ (June 2017). "Prevention, treatment, and rehabilitation of anterior cruciate ligament injuries in children". Open up Admission Journal of Sports Medicine. eight: 133–141. doi:ten.2147/OAJSM.S133940. PMC5476725. PMID 28652828.
- ^ Dekker TJ, Godin JA, Dale KM, Garrett We, Taylor DC, Riboh JC (June 2017). "Return to Sport After Pediatric Anterior Cruciate Ligament Reconstruction and Its Effect on Subsequent Anterior Cruciate Ligament Injury". The Journal of Os and Joint Surgery. American Book. 99 (11): 897–904. doi:10.2106/JBJS.16.00758. PMID 28590374. S2CID 46577033.
- ^ Boden BP, Sheehan FT, Torg JS, Hewett TE (September 2010). "Noncontact anterior cruciate ligament injuries: mechanisms and chance factors". The Journal of the American Academy of Orthopaedic Surgeons. eighteen (9): 520–7. doi:ten.5435/00124635-201009000-00003. PMC3625971. PMID 20810933.
- ^ Myer GD, Sugimoto D, Thomas S, Hewett TE (January 2013). "The influence of historic period on the effectiveness of neuromuscular grooming to reduce inductive cruciate ligament injury in female person athletes: a meta-analysis". The American Journal of Sports Medicine. 41 (one): 203–xv. doi:10.1177/0363546512460637. PMC4160039. PMID 23048042.
- ^ a b Lopes, Thiago Jambo Alves; Simic, Milena; Myer, Gregory D.; Ford, Kevin R.; Hewett, Timothy E.; Pappas, Evangelos (May 2018). "The Effects of Injury Prevention Programs on the Biomechanics of Landing Tasks". The American Journal of Sports Medicine. 46 (half-dozen): 1492–1499. doi:x.1177/0363546517716930. ISSN 0363-5465. PMC6604048. PMID 28759729.
- ^ Filbay SR, Grindem H (February 2019). "Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture". Best Practice & Inquiry. Clinical Rheumatology. 33 (1): 33–47. doi:10.1016/j.berh.2019.01.018. PMC6723618. PMID 31431274.
- ^ Ihara H, Kawano T (2017). "Influence of Age on Healing Capacity of Astute Tears of the Inductive Cruciate Ligament Based on Magnetic Resonance Imaging Assessment". Journal of Estimator Assisted Tomography. 41 (2): 206–211. doi:10.1097/RCT.0000000000000515. PMC5359784. PMID 28045756.
- ^ Järvelä T, Moisala AS, Sihvonen R, Järvelä S, Kannus P, Järvinen One thousand (Feb 2008). "Double-parcel anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference spiral fixation: prospective, randomized, clinical study with 2-twelvemonth results". The American Journal of Sports Medicine. 36 (ii): 290–7. doi:10.1177/0363546507308360. PMID 17940145. S2CID 25213872.
- ^ Bottoni CR, Liddell TR, Trainor TJ, Freccero DM, Lindell KK (April 2008). "Postoperative range of motion following inductive cruciate ligament reconstruction using autograft hamstrings: a prospective, randomized clinical trial of early versus delayed reconstructions". The American Journal of Sports Medicine. 36 (4): 656–62. doi:x.1177/0363546507312164. PMID 18212347. S2CID 36355558.
- ^ "OrthoGuidelines". Retrieved 23 March 2018.
- ^ Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ (Nov 2014). "Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment". The American Periodical of Sports Medicine. 42 (11): 2769–76. doi:ten.1177/0363546513510889. PMID 24305648. S2CID 1313316.
- ^ Dunn KL, Lam KC, Valovich McLeod TC (May 2016). "Early Operative Versus Delayed or Nonoperative Treatment of Anterior Cruciate Ligament Injuries in Pediatric Patients". Journal of Athletic Preparation. 51 (five): 425–7. doi:ten.4085/1062-6050.51.v.xi. PMC5013703. PMID 27244126.
- ^ Mall NA, Chalmers PN, Moric Chiliad, Tanaka MJ, Cole BJ, Bach BR, Paletta GA (Oct 2014). "Incidence and trends of inductive cruciate ligament reconstruction in the United States". The American Journal of Sports Medicine. 42 (x): 2363–seventy. doi:ten.1177/0363546514542796. PMID 25086064. S2CID 24764031.
- ^ Hughes, Gerwyn; Musco, Perry; Caine, Samuel; Howe, Lauren (2020-08-01). "Lower Limb Asymmetry Afterwards Anterior Cruciate Ligament Reconstruction in Adolescent Athletes: A Systematic Review and Meta-Assay". Journal of Athletic Grooming. 55 (8): 811–825. doi:10.4085/1062-6050-0244-19. ISSN 1938-162X. PMC7462171. PMID 32607546.
- ^ "Anterior Cruciate Ligament Injury". Retrieved 23 March 2018.
- ^ Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, Hewett TE (October 2010). "Biomechanical measures during landing and postural stability predict second inductive cruciate ligament injury after anterior cruciate ligament reconstruction and render to sport". The American Journal of Sports Medicine. 38 (ten): 1968–78. doi:ten.1177/0363546510376053. PMC4920967. PMID 20702858.
- ^ a b Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, et al. (June 2016). "Incidence of Inductive Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Written report". The American Journal of Sports Medicine. 44 (six): 1502–7. doi:10.1177/0363546516629944. PMID 26920430. S2CID 36050753.
- ^ Gans I, Retzky JS, Jones LC, Tanaka MJ (June 2018). "Epidemiology of Recurrent Anterior Cruciate Ligament Injuries in National Collegiate Athletic Association Sports: The Injury Surveillance Program, 2004-2014". Orthopaedic Journal of Sports Medicine. 6 (6): 2325967118777823. doi:x.1177/2325967118777823. PMC6024527. PMID 29977938.
- ^ a b Ireland ML, Gaudette M, Crook Due south (May 1997). "ACL Injuries in the Female person Athlete". Journal of Sport Rehabilitation. half-dozen (two): 97–110. doi:10.1123/jsr.six.2.97.
- ^ Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ (Oct 2016). "Sport-Specific Yearly Run a risk and Incidence of Anterior Cruciate Ligament Tears in High Schoolhouse Athletes: A Systematic Review and Meta-analysis". The American Journal of Sports Medicine. 44 (ten): 2716–2723. doi:10.1177/0363546515617742. PMID 26657853. S2CID 23050724.
- ^ Engdahl, Karolina; Emanuelson, Ulf; Höglund, Odd; Bergström, Annika; Hanson, Jeanette (Dec 2021). "The epidemiology of cruciate ligament rupture in an insured Swedish dog population". Scientific Reports. 11 (one): 9546. doi:10.1038/s41598-021-88876-3. PMC8100293.
External links [edit]
Source: https://en.wikipedia.org/wiki/Anterior_cruciate_ligament_injury
Posted by: lazarusfround.blogspot.com


0 Response to "Can A Torn Acl Be Repaired"
Post a Comment